According to NAMI, any traumatic event can trigger a psychotic episode. Car accidents. War. Violent assaults. Terrorism. Physical abuse. Sexual abuse or extreme neglect. However, certain events are more highly linked to psychosis. Experiencing a natural disaster and seeing someone killed or injured are both traumas that have been shown to induce psychosis in many people.
Childhood Trauma and Psychosis
Additionally, childhood trauma—particularly childhood sexual abuse— has received a lot of attention for its connection to psychosis.
One study on almost 100 Los Angeles teens with psychosis showed that most of them suffered through sexual abuse as children. These teens were all homeless, living on the streets. The teens who were abused as kids were more likely to hear things, though they also reported symptoms of paranoia. Childhood sexual abuse is thus a significant predictor for auditory hallucinations (Mundy, 1990).
In another study of about 8500 adults, those who had symptoms of psychosis were significantly more likely to have experienced trauma as children. (Bebbington, 2004).
The Relationship Between Teen PTSD and Psychosis
Post-traumatic stress disorder and psychosis often go hand in hand. PTSD can involve psychosis—hallucinations, delusions, and the negative symptoms like flat affect and emotional in-expression. The symptoms for both PTSD and psychosis can thus overlap.
In one study of almost 6000 people in the U.S. more than half of the participants who had PTSD also reported experiencing a psychotic symptom. The most common symptom was the delusion that other people were spying on them. Almost 30% of participants felt that they were being followed by others.
Why Does Trauma Lead to Psychosis?
Some believe that psychotic symptoms are a “coping mechanism” for the traumatic event one has experienced. Award-winning author and public speaker Eleanor Longden, who shared her experience with schizophrenia in a widely publicized TED Talk, feels this way. She says the voices she hears inside her head are “a survivors’ strategy, a sane reaction to insane circumstances.”
The Stress Vulnerability Model
However, it’s important to mention that while trauma may result in psychotic symptoms, many people experience traumatic incidents and are not diagnosed with psychosis or schizophrenia (the most common mental health disorder involving psychosis).
Lauren Cona, Clinical Program Director at Evolve Woodland Hills, a teen mental health treatment facility in Los Angeles, says the way to understand this is through the “stress vulnerability model” (Zubin, 1977).
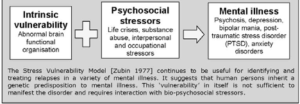
“Alcohol or drug use, biological pre-disposal, coping skills for managing stress, emotional and physical health, family and social support…all of these factors can contribute to risk for psychosis. So, if an adolescent has family and friends in their support system, is involved in meaningful activities, has learned coping skills to deal with everyday challenges, and abstains from substances, these things can result in better mental health outcomes. Teens who don’t have consistent supports in place may be more vulnerable to severe mental health challenges.”
Treatment for Teen Trauma or PTSD
If you know, or believe, that your child has suffered a trauma, it’s important to get help right away. Early treatment after a traumatic incident, as well as self-care and learning the proper coping skills to deal with said trauma, can limit and even prevent further suffering in the form of psychosis.






